Asbestos is a naturally occurring mineral that can be harmful to human health due to its carcinogenic nature. However, if asbestos is such a dangerous element, why did people use it from the 1950s to the 1970s inside their homes? Well, it was due to its heat-proof qualities.
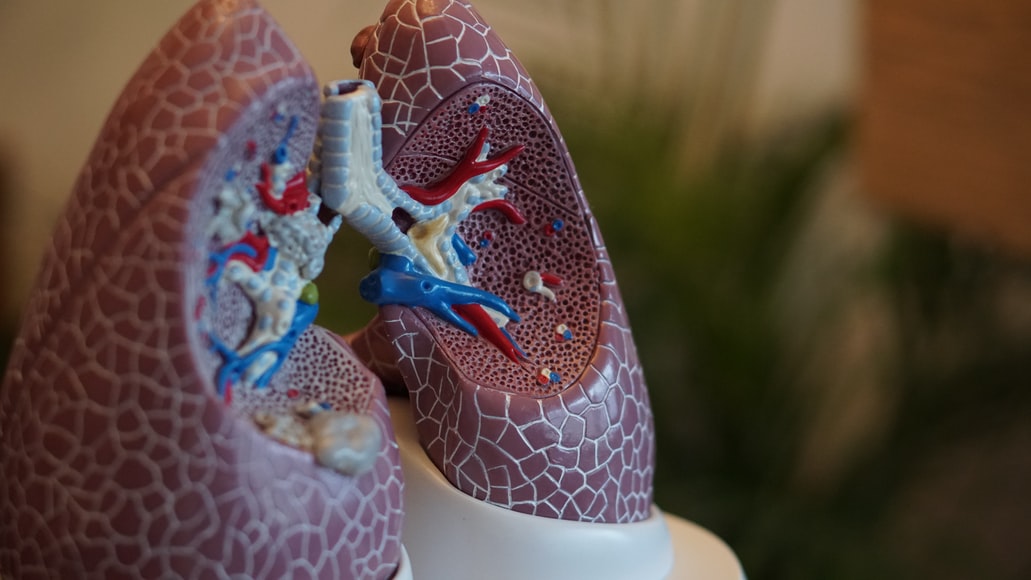
Typically, asbestos was used as insulation material inside houses. However, asbestos can cause various diseases, one of which is mesothelioma. It is a form of cancer that results from prolonged exposure to asbestos. It usually occurs when you breathe in asbestos fibers, leading to a malignant cancerous growth on the lining of your lungs.
Some symptoms might include but are not limited to high-grade fever, respiratory issues, muscle weakness, shortness of breath, dry coughing, and much more.
Finding out that you have mesothelioma can be devastating. That doesn’t mean they should give up hope and count the days they have left to live. Sure, no amount of money will help you improve your mental well-being. However, compensation will enable you to pay for treatment or ensure that your family is well-cared for. That being said, let us look at a few steps you can take if you end up developing mesothelioma.
Research Your Treatment Options
While it may be impossible to reverse the lung damage caused by this type of cancer, you still have a few treatment options after contracting mesothelioma. For instance, if you contract pleural mesothelioma, some treatment options include chemotherapy, radiation therapy, and surgery.
These treatment options will help slow down the spread of cancer and alleviate some symptoms. Furthermore, doctors might ask you to undergo oxygen therapy to help you breathe easier if your lungs are damaged due to mesothelioma. Plus, they might also suggest you quit smoking to prevent further damage.
The effectiveness of treatment will depend on the stage of cancer. For instance, if your mesothelioma is at its second or third stage, your physician might recommend chemo or radiotherapy as a last resort.
Consult With Your Primary Care Physician
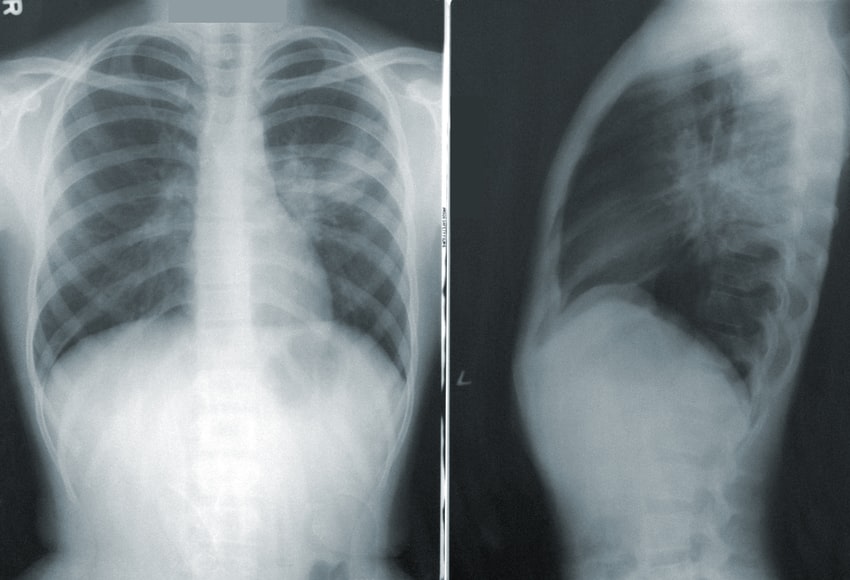
Once you’ve researched all your treatment options, talking to your primary care physician about which one is right for you is the next step to take. Your doctor will assess your cancer and provide you with a better idea of what treatment option will be the best fit for you.
However, the good news is that sometimes, the symptoms might be due to another medical issue altogether. After all, mesothelioma results from years of asbestos exposure, and symptoms probably won’t show up until fifteen to twenty years after exposure.
So, it would be wise to consult your doctor to rule out all other medical conditions that have similar symptoms as mesothelioma. However, if you’re already diagnosed with this type of cancer, your primary care physician will keep you under observation and refer you to a pulmonologist.
Hire A Mesothelioma Attorney
If your doctor has diagnosed your cancer, the next step is to hire a competent mesothelioma attorney. A mesothelioma lawyer will help you file your lawsuit on time. That said, there are two types of mesothelioma lawsuits that you can file; a personal injury and a wrongful death claim. In the case of a personal injury lawsuit, your mesothelioma lawyer will help you file a claim for compensation against your employer.
However, you will be eligible for this type of claim if you can provide information about your diagnoses like employment records, medical reports, evidence of exposure at your workplace, and much more. So, go ahead and hire a competent mesothelioma lawyer if you think that your diagnosis was a direct result of asbestos exposure at your workplace.
Search For A Support Network
There is no shadow of a doubt that a mesothelioma diagnosis will affect your physical, mental, and emotional well-being. So, searching for a support network for family and friends is vital for recovery. After all, it would help immensely to never feel disheartened and alone after receiving your diagnosis.
If you don’t have any friends or family members to confide in, look for an oncology cancer social worker. They will guide you and help you search for resources to manage your mesothelioma effectively.
In addition, signing up for a cancer support group is another viable option. In fact, you can go online and search for such support groups with the click of a mouse.
Being diagnosed with mesothelioma will undoubtedly leave you in a state of emotional turmoil. While the steps mentioned in this article will allow you to improve your quality of life, don’t forget to prioritize spending time with your friends, family, and loved ones!
So, go ahead and surround yourself with people who will support you and love you during such a testing time of your life. not to mention, leaning on loved ones for help and support will enable you to stay motivated and keep a positive look on life.
Read Also: